To help celebrate Food Allergy Awareness week, I asked my followers on social media to tell me what they would like to hear about. Due to so many requests, I decided to answer questions throughout the whole month of May. The last request I received was about food allergies and asthma. I am not equipped to answer this question myself, but I am thankful that I know someone who is. Last week I introduced you all to Dr. Ana-Maria Temple who is a pediatrician. She is a wealth of information and has kindly written a two part series for all of us on this important topic. Her and I decided to do this in two parts because there is so much information that we would like you all to have. This week Ana-Maria will be teaching us about food allergies and their affect on asthma. Next Friday, she will be teaching us about how to prevent asthma and also functional medicine treatments for asthma. Be sure to come back next week. Thank you Ana-Maria for everything you do to educate us!
The Relationship between Food Allergies and Asthma
There is a close relationship between asthma and food allergies, though the actual relationship is
not yet fully understood. Here is what we know so far based on the latest medical
literature.
General Information:
• Asthma and food allergy may often coexist.
• Up to 45% of children with asthma have food sensitivity by food sIgE.
• Food-allergic children were found to have 29% chance of having asthma by the US National
Center for Health Services (NCHS)
• Food allergic individuals with asthma are at higher risk for severe asthma then individuals
that have asthma and no food allergies.
• Food allergic individuals with asthma are at a higher risk for severe allergic reactions to
foods, particularly if the asthma is uncontrolled.
• Children with asthma and food allergies are less likely to outgrow their food allergies, then
those with only food allergies.
• Food allergy should be considered in children with acute life-threatening asthma
exacerbations with no identifiable triggers.
• Food allergy should be considered in children with moderate to severe eczema and with
severe persistent asthma. (Editorial note: I would consider this connection even in
children with mild to moderate eczema and asthma combo)
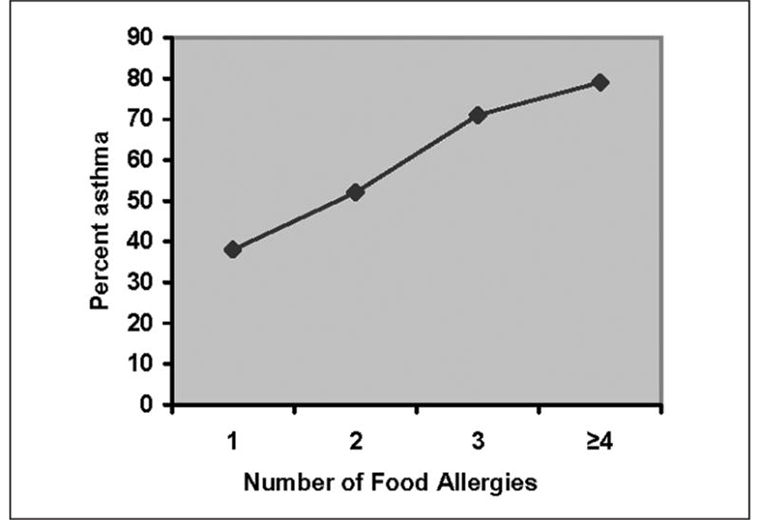
• Being sensitive to more foods and having higher levels of sensitization is associated with
increased severity of asthma. See Photo Above
• Food allergies often affect young children, can develop before the onset of asthma, and are
considered a risk factor for persistent, problematic asthma in young children.
• Studies indicate that children with food allergy present with asthma at an earlier age than
those without a history of food allergy.
Looking at Individual Foods:
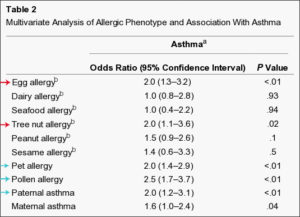
Table outlining the foods that have the highest association with the development of Asthma
(red). Blue arrows show the other factors associated with increased risk of
developing Asthma.
• Sensitization to egg, one of the most common food allergens in childhood, has been shown to
be a risk factor for developing environmental allergens and asthma later in life
• A specific study examined the role of clinical peanut allergy with asthma. The authors
reported that having peanut allergy (based on a positive history of reactions, peanut-
specific IgE > 15 kU/L and positive skin test to peanut) was associated with increased
rates of hospitalization and use of systemic steroids as compared to asthmatics
without peanut allergy.
• A 2009 study found that having cow’s milk allergy is a predictor for subsequent airway
inflammation. Children with IgE-mediated milk allergy at 7 months of age diagnosed
by oral food challenge had increased risk of elevated airway inflammation at 8 years
of age.
• The presence of asthma is a predictor for persistent cow’s milk allergy
• Wheezing infants, who have test for specific IgE of >or=0.35 kU/L to wheat, egg white, or
environmental allergens are at higher risk for developing asthma later in childhood.
Consequently, detection of those specific IgE antibodies in wheezing infants may help
with the early diagnosis of asthma, especially in cases with no clinically evident
eczema.
A Word of Caution:
• Cross-reactivity between foods and environmental allergens can lead to positive skin tests or
serum IgE levels to foods that may not be clinically relevant. For example, people
with birch tree pollen allergies can test positive to peanut and those with dust mite
and/or cockroach allergies can test positive to shrimp
In Good Health, Ana-Maria Temple, MD
Citations:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3155248/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2990684/
https://www.ncbi.nlm.nih.gov/pubmed/20146729
https://www.ncbi.nlm.nih.gov/pubmed/12859453
https://www.ncbi.nlm.nih.gov/pubmed/10981525
https://www.ncbi.nlm.nih.gov/pubmed/16210063
https://www.ncbi.nlm.nih.gov/pubmed/17469157
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2922978/
https://www.ncbi.nlm.nih.gov/pubmed/20618346
https://www.ncbi.nlm.nih.gov/pubmed/12612281
https://www.ncbi.nlm.nih.gov/pubmed/15867869
https://www.ncbi.nlm.nih.gov/pubmed/19389315
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3070157/ – charts authors